What Are Peptides: Understanding These Molecular Messengers
A science-based guide to understanding peptide function, safety, and real-world applications

If you've browsed skincare labels, scrolled through fitness forums, or explored wellness trends lately, you've probably encountered peptides. These molecules have moved from laboratory obscurity into mainstream conversation, appearing in everything from anti-aging creams to therapeutic discussions. But cutting through the marketing noise to understand what peptides actually are requires looking at the biochemistry.
The Basic Chemistry of Peptides
A peptide consists of amino acids joined by peptide bonds. The distinction between peptides and proteins comes down to size: peptides contain between 2 and 50 amino acids, while proteins contain 50 or more. This isn't just semantic splitting. The smaller size of peptides affects how they behave in biological systems, how quickly they're absorbed, and what functions they can perform.
When two amino acids link together, they form a dipeptide. Three create a tripeptide. Longer chains fall into the category of polypeptides. The sequence matters enormously. Changing even one amino acid in the chain can completely alter what the peptide does or whether it works at all.
Your body produces peptides constantly. Hormones like insulin and oxytocin are peptides. The endorphins that reduce pain perception are peptides. Antibodies that fight infection contain peptide structures. These molecules act as messengers, carrying signals between cells and triggering specific biological responses.
How Peptides Function in the Body
Peptides work through receptor binding. Each peptide has a three-dimensional shape determined by its amino acid sequence. This shape allows it to fit into specific receptors on cell surfaces, much like a key entering a lock. When binding occurs, the cell receives instructions to start or stop certain processes.
The peptide bond itself forms through dehydration synthesis. The carboxyl group of one amino acid connects to the amino group of another, releasing a water molecule. This creates the backbone structure that gives peptides their stability and function.
Not all peptides last long in the body. Enzymes called peptidases break down peptides into their component amino acids. Some peptides degrade within minutes, while others remain active longer. This variability has driven research into peptide modifications that resist enzymatic breakdown, extending their therapeutic window.
Once you understand how peptides work in the body, the next step is making sure your dosage is accurate. You can calculate your peptide dosage precisely using our peptide calculator, which accounts for vial strength, reconstitution volume, and target dosing.
If you want a deeper understanding of how peptide dosages are calculated, including common conversion errors to avoid, see our peptide dosage calculation guide, which walks through the logic step by step.
Categories of Peptides and Their Roles
Signal Peptides
These molecules tell cells what to do. In skin, certain signal peptides stimulate fibroblasts to produce collagen and elastin, proteins that maintain structural integrity. The cosmetics industry has invested heavily in signal peptides, though their effectiveness depends on molecular weight, formulation, and penetration through the stratum corneum.
Carrier Peptides
Carrier peptides transport trace elements to where cells need them. Copper peptides, for instance, deliver copper ions that participate in wound healing and collagen synthesis. The research supporting topical copper peptides dates back decades, with studies showing effects on skin repair and appearance.
Enzyme Inhibitors
Some peptides block enzymes that break down structural proteins. Matrix metalloproteinases (MMPs) degrade collagen and elastin during natural aging and photo-damage. Peptides that inhibit MMPs may slow this breakdown, though the degree of effect in topical applications remains under investigation.
Neuropeptides
These peptides affect nerve signaling. Substance P transmits pain signals. Endorphins modulate pain and mood. Neuropeptide Y influences appetite and stress responses. Understanding these molecules has opened therapeutic avenues for pain management and neurological conditions.
Medical Applications of Peptides
Peptide-based drugs have been used clinically for nearly a century. Insulin, discovered in 1921, revolutionized diabetes treatment and remains a cornerstone therapy. Modern pharmaceutical development has produced peptide drugs for conditions
including osteoporosis, cancer, and infectious disease.
Growth hormone-releasing peptides (GHRPs) stimulate the pituitary gland to release growth hormone. Medical interest in these compounds centers on conditions involving growth hormone deficiency. Applications outside approved medical uses enter legally and ethically complex territory, particularly regarding athletic performance.
Thymosin alpha-1, a peptide originally isolated from thymus tissue, has been studied for immune modulation. Research has examined its potential in treating hepatitis, cancer, and immunodeficiency, though clinical adoption varies by country and indication.
Antimicrobial peptides represent a promising area as antibiotic resistance grows. These molecules, part of innate immune defense, can kill bacteria through membrane disruption rather than the mechanisms bacteria have learned to resist. Clinical development faces challenges including stability, delivery, and manufacturing costs.
Peptides in Performance and Body Composition
Athletes have shown sustained interest in peptides that might enhance recovery, increase muscle mass, or improve performance. Growth hormone secretagogues have received particular attention for their potential effects on lean body mass and fat distribution.
BPC-157, a synthetic peptide derived from a protein found in gastric juice, has been studied primarily in animal models for tissue repair and healing. TB-500, a synthetic version of thymosin beta-4, has similarly been investigated for wound healing and tissue regeneration. Human clinical trials for these peptides remain limited, and most evidence comes from animal studies or anecdotal reports.
The World Anti-Doping Agency prohibits many peptides in competitive sports, classifying them under growth hormone secretagogues and peptide hormones. Athletes considering peptide use face both regulatory consequences and health risks from unverified products.
Collagen peptides taken orally have shown some evidence for supporting joint health and skin appearance in clinical trials. These hydrolyzed proteins are broken down into smaller peptides that may be absorbed intact and incorporated into connective tissue, though the mechanisms remain under study.
Understanding Peptide Safety and Regulation
The peptide market exists in multiple regulatory spaces. FDA-approved peptide drugs undergo rigorous testing for safety and efficacy. Peptides from compounding pharmacies occupy a different category, with less oversight. Research-grade peptides sold for laboratory use carry explicit warnings against human consumption.
The Research-Grade Distinction
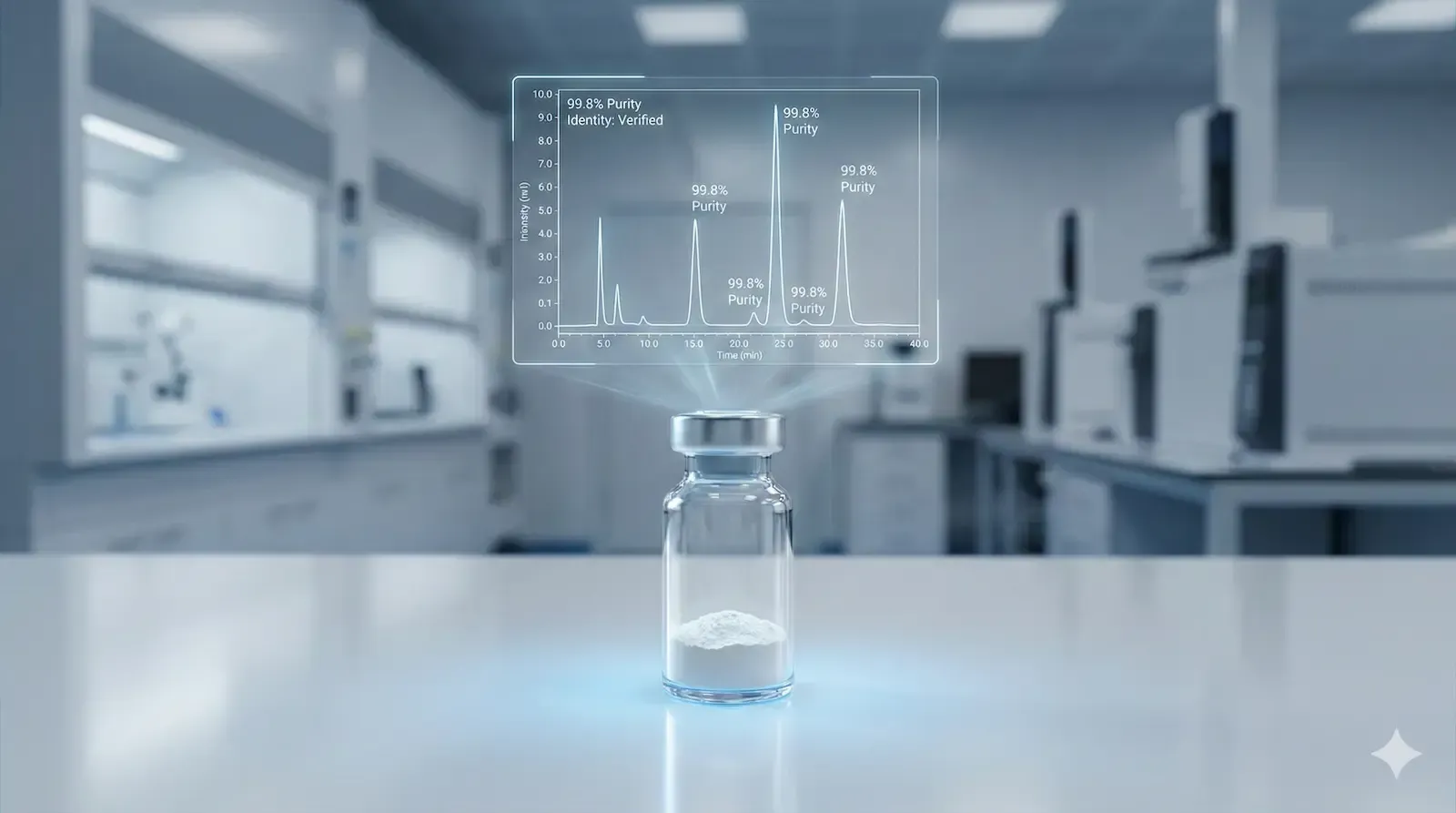
Research-grade peptides are manufactured for scientific investigation, not clinical use. They lack the purity standards, sterility testing, and quality controls required for pharmaceuticals.
Can doctors prescribe research-grade peptides?
No. Medical professionals can only prescribe pharmaceutical-grade compounds approved for human use or obtained through licensed compounding pharmacies for specific therapeutic purposes.
Using research chemicals outside controlled laboratory settings violates federal law and poses serious health risks. Contamination, incorrect concentration, and presence of toxic byproducts can occur in products not manufactured to pharmaceutical standards.
Quality varies dramatically across peptide sources. Third-party testing for purity and composition provides some assurance, but even tested products may not match pharmaceutical-grade standards. Adverse reactions from contaminated or mislabeled peptides have been documented, including infections from non-sterile injectable formulations.
Current Research Directions
Peptide research has accelerated as techniques for synthesis and modification have advanced. Chemical modifications can improve stability, enhance receptor selectivity, and extend half-life. PEGylation, where polyethylene glycol is attached to a peptide, can protect it from enzymatic degradation and reduce clearance rates.
Delivery methods continue evolving. Oral peptide drugs have traditionally faced challenges because digestive enzymes break them down before absorption. Protective formulations and chemical modifications are improving oral bioavailability for some peptides. Nasal sprays, transdermal patches, and sublingual delivery offer alternatives to injection.
Peptide vaccines represent an active research area. Unlike traditional vaccines that use whole pathogens or inactivated viruses, peptide vaccines use specific peptide sequences from disease-causing organisms to trigger immune responses. This approach may offer advantages in safety and manufacturing scalability.
Cancer immunotherapy has incorporated peptides in various ways. Some approaches use tumor-associated peptides to train the immune system to recognize cancer cells. Others employ peptides to block signals that tumors use to evade immune detection. Clinical results have been mixed, with some peptide vaccines showing promise while others have failed to demonstrate efficacy in large trials.
Peptides in Skincare: What the Evidence Shows
The skincare industry has embraced peptides enthusiastically, but scientific support varies by peptide type and formulation. Molecular weight affects whether peptides can penetrate the stratum corneum, the skin's outer barrier. Smaller peptides may penetrate better, but size alone doesn't guarantee effectiveness.
Palmitoyl pentapeptide (Matrixyl) has been studied in several clinical trials for anti-aging effects. Results have shown improvements in fine lines and wrinkles, though effect sizes are modest compared to retinoids or prescription treatments. Copper peptides have demonstrated wound-healing properties in clinical settings, and some evidence supports their use in cosmetic formulations.
Marketing claims often outpace scientific evidence. Terms like "clinically proven" may refer to small, non-peer-reviewed studies. Peptide concentration matters, but manufacturers rarely disclose specific amounts. Formulation stability presents another challenge since peptides can degrade in certain pH ranges or when exposed to light.
Making Informed Decisions About Peptide Use
Anyone considering peptide therapy should start with medical consultation. Healthcare providers can assess whether peptides might benefit specific conditions and determine appropriate options. Blood work, medical history, and current medications all factor into safety considerations.
Verifying product legitimacy matters. Pharmaceutical-grade peptides come through licensed medical channels with clear documentation. Products from unregulated sources may not contain what labels claim. Testing and verification add costs but provide critical quality assurance.
Expectations should align with evidence. Peptides are not cure-alls despite marketing language suggesting otherwise. Medical applications with strong evidence, like insulin for diabetes, differ substantially from speculative uses lacking clinical validation.
Understanding this distinction helps separate legitimate therapeutic applications from overhyped wellness trends. Cost varies widely. Prescription peptide therapies through medical providers typically involve clinical monitoring and pharmaceutical-grade products. Unregulated alternatives may seem cheaper initially but carry risks that can result in greater expense through adverse effects or ineffective treatment.
The Broader Context of Peptide Science
Peptide research intersects with multiple scientific fields. Proteomics, the large-scale study of proteins, has revealed thousands of naturally occurring peptides in human biology, many with unknown functions. As analytical techniques improve, researchers continue discovering peptides with potential therapeutic applications.
The human body produces antimicrobial peptides as part of innate immunity. These molecules provide first-line defense against pathogens on skin and mucous membranes. Understanding how these natural peptides work has informed development of synthetic antimicrobial compounds.
Plant and animal sources provide peptides with biological activity. Venoms contain peptides that affect nerve transmission and blood clotting, some of which have been developed into drugs. Marine organisms produce peptides that researchers are investigating for various applications. This bioprospecting has identified novel peptide structures with therapeutic potential.
Practical Considerations for Peptide Applications
Storage requirements for peptides depend on their stability. Many peptide formulations require refrigeration. Freeze-thaw cycles can degrade some peptides. Reconstituted peptides often have limited shelf lives once mixed. Following storage guidelines preserves potency and prevents premature breakdown.
Administration routes affect absorption and bioavailability. Injectable peptides typically show higher bioavailability than oral forms. Subcutaneous injection allows sustained release, while intravenous administration provides rapid delivery. Topical application works for some peptides but depends heavily on molecular characteristics and formulation.
Timing and dosing protocols vary by peptide and application. Some peptides work best when taken at specific times relative to meals or sleep. Others require multiple daily doses. Medical oversight ensures appropriate protocols for therapeutic applications.
Monitoring responses helps gauge effectiveness and identify problems. Depending on the peptide and condition, monitoring might include blood tests, symptom tracking, or imaging studies. Adjustment of dosing or discontinuation may be necessary based on response and side effects.
The Intersection of Peptides and Personalized Medicine
Genetic variations affect how individuals respond to peptides. Differences in receptor expression, enzyme activity, and metabolism can influence both effectiveness and side effect profiles. As genetic testing becomes more accessible, tailoring peptide therapy to individual genetic profiles may become more common.
Peptide biomarkers are being developed for disease diagnosis and monitoring. These naturally occurring peptides in blood or tissue can indicate disease states, treatment response, or prognosis. B-type natriuretic peptide (BNP), for instance, helps assess heart failure severity.
The concept of peptide libraries involves creating large collections of peptide variants to screen for desired properties. This approach has accelerated drug discovery by allowing researchers to test thousands of peptide variations against biological targets.
**Source Quality Peptides with Confidence**
If you're working with a qualified provider on peptide therapy, sourcing matters. Project Biohacking has partnered with peptide suppliers that provide certificates of analysis, third-party testing, and proper quality controls.
View our trusted vendor partners → (https://www.projectbiohacking.com/resources/vendor)
Save 15% with exclusive discount codes:
- **Limitless Biotech**: Use code PROBIO15
- **Biolongevity Labs**: Use code PROBIO15
- **CanLab International**: Use code PROBIO15
Always consult your healthcare provider before using any peptide or supplement.
FAQ
What is a peptide?
A peptide is a chain of amino acids connected by peptide bonds, containing between 2 and 50 amino acids. These molecules function as signaling agents in the body, instructing cells to perform specific actions. Your body naturally produces thousands of different peptides that regulate hormones, support immune function, and facilitate tissue repair. Synthetic peptides are manufactured for medical, cosmetic, and research purposes.
What is the main difference between a peptide and a protein?
Size determines the distinction. Peptides contain 2 to 50 amino acids, while proteins consist of 50 or more amino acids arranged in complex three-dimensional structures. Peptides are generally simpler molecules with more targeted functions. Proteins perform broader structural and functional roles, such as forming muscle tissue or transporting oxygen in blood. Both are built from amino acids, but their size difference affects their biological behavior.
Are peptides safe to use?
Safety depends on which peptide, its source, purity level, and how it's used. FDA-approved peptide medications prescribed by doctors undergo rigorous testing and quality control. Research-grade peptides sold for laboratory use are not safe for human consumption due to lack of purity standards and sterility testing. Peptides from unregulated sources may contain contaminants or incorrect concentrations. Medical supervision is necessary for any peptide therapy to monitor for side effects and ensure proper dosing.
Can doctors prescribe research grade peptides?
No. Research-grade peptides are manufactured exclusively for laboratory investigation and carry explicit warnings against human use. Doctors can only prescribe pharmaceutical-grade peptides approved by regulatory agencies or obtained through licensed compounding pharmacies for legitimate medical purposes. Using research chemicals outside controlled laboratory settings violates federal regulations and poses serious health risks including contamination, infection, and toxic reactions from impurities.
How do peptides work in skincare products?
Peptides in skincare penetrate the outer layer of skin and bind to receptors on skin cells, signaling them to increase collagen production or perform other functions. Signal peptides stimulate collagen synthesis, carrier peptides deliver minerals like copper to cells, and enzyme inhibitor peptides block proteins that break down collagen. Effectiveness depends on the peptide's molecular weight, concentration, formulation stability, and ability to penetrate skin barriers. Clinical evidence varies considerably among different peptide types.
What medical conditions can peptides treat?
FDA-approved peptide medications treat diabetes (insulin), osteoporosis (calcitonin), growth hormone deficiency, and certain cancers. Other peptides are being investigated for immune disorders, wound healing, and chronic inflammatory conditions, though these applications remain largely experimental. The specific medical uses depend on the individual peptide and whether it has received regulatory approval. Many claimed therapeutic benefits lack sufficient clinical evidence from human trials.
How long before peptides show results?
Timeline varies by peptide type and application. Topical skincare peptides may show subtle improvements after 4 to 8 weeks of consistent use, with more noticeable results taking several months. Therapeutic peptides for medical conditions might produce effects within days to weeks depending on the condition being treated. Peptides aimed at body composition or athletic performance could require 8 to 12 weeks before changes become apparent. Individual response varies based on genetics, overall health, dosing, and administration method.
**Disclaimer**
**Medical Information:**
This article provides educational information only and should not be considered medical advice, diagnosis, or treatment recommendations. The content is based on scientific research and consensus knowledge available as of the publication date. Always consult a licensed healthcare provider before starting any peptide therapy, supplement regimen, or health intervention.
**No Professional Relationship:**
Reading this article does not create a healthcare provider-patient relationship. Individual health circumstances vary, and what works for one person may not be appropriate for another.
**Product Quality:**
References to specific peptides, brands, or vendors are for informational purposes. We do not guarantee the safety, efficacy, or legality of any products. Users assume all responsibility for product selection and use.
**Affiliate Disclosure:**
Project Biohacking participates in affiliate partnerships and may receive commissions from purchases made through our links at no additional cost to you. Use all information and products at your own risk.