How to Take a Peptide Shot (Step-by-Step Guide)
What “Taking a Peptide Shot” Usually Means

Educational only, not medical advice. Always follow your licensed clinician’s instructions for dose, route (SubQ vs IM), timing, storage, and technique.
Peptide shots(peptide injections) can be part of a provider-guided wellness plan, but the benefits only matter if your process is clean, consistent, and accurate. Most injection issues come from rushing, sloppy technique, or “winging it” based on what’s trending online.
Project Biohacking is built around a simple idea: turn complicated science into clear action—without hype. If you’ve been prescribed an injectable peptide and your clinician has trained you to self-administer, this guide walks you through the practical “how-to” fundamentals.
Most at-home peptide injections are subcutaneous (SubQ), meaning the peptide is injected into the fatty layer just under the skin. SubQ is common because it’s typically easier to learn, uses smaller needles, and is generally well tolerated once you’re trained.
Less commonly, a provider may direct intramuscular (IM) injections (into muscle). IM requires different needle selection and technique. If your prescription says IM and you haven’t been trained hands-on, stop and ask your provider for guidance.
If you want a deeper overview of what peptide therapy is (and why delivery method matters), start here: Peptide Therapy Explained.
Before You Inject: 60-Second Safety Checklist
- Confirm route + dose: You should know exactly what you’re injecting, how much, and whether it’s SubQ or IM.
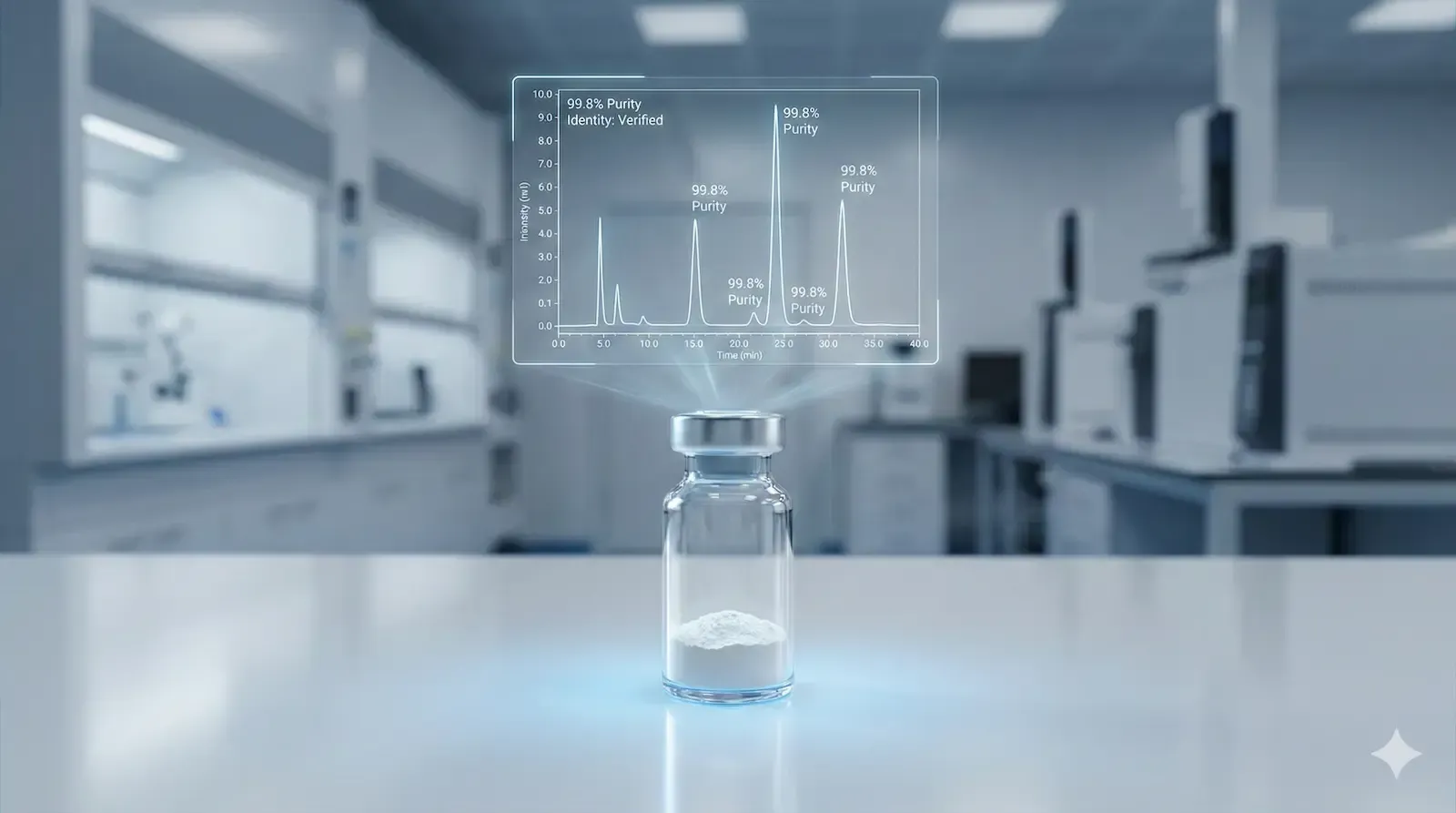
- Inspect the medication: Don’t inject if a vial is cracked, the seal is broken, the solution looks questionable, or anything seems “off.”
- Check storage requirements: Many peptides are temperature-sensitive. Follow the pharmacy label.
- Don’t improvise: No dosage “freestyling” and no protocol changes without your clinician.
Get urgent medical help if you experience trouble breathing, swelling of face/lips/tongue/throat, widespread hives, or symptoms of a severe allergic reaction. Also seek care for rapidly worsening redness, heat, swelling, pus/drainage, or fever (possible infection).
What You’ll Need
Most SubQ peptide shots require the following:
- Prescribed peptide medication (prefilled syringe or vial)
- New sterile syringe/needle (if not prefilled)
- Alcohol swabs
- Clean gauze or cotton pad
- Sharps container (puncture-resistant)
- Optional: small bandage
If your peptide is a powder that requires mixing (reconstitution): do that only if you’ve been instructed and trained. For step-by-step reconstitution basics, see: Peptide Reconstitution Guide. If you’re learning what bacteriostatic water is and why it’s used, read: Bacteriostatic Water for Peptides.
Step-by-Step: How to Take a Peptide Shot (SubQ)
Step 1) Set up a clean, calm workspace
- Wash your hands with soap and water for 20 seconds.
- Use a clean, well-lit surface (no clutter, no distractions).
- Lay out everything you need before you start.
Why it matters: Most injection errors happen before the needle touches skin—rushing, contamination, or forgetting supplies mid-process.
Step 2) Verify the label every time
Confirm:
- Medication name
- Concentration (if applicable)
- Route (SubQ vs IM)
- Expiration date
- Storage instructions
If anything doesn’t match what you were prescribed, stop and contact your pharmacy or provider.
Step 3) Choose the injection site (and rotate)
Common SubQ sites include:
- Abdomen: avoid a 2-inch circle around the belly button
- Outer thigh
- Back/side of upper arm(often easier if someone helps)
Rotate sites to reduce irritation, bruising, and the chance of developing tender lumps over time. Avoid injecting into bruised, scarred, hard/lumpy, red, or inflamed areas.
Note on “knee injections”: If a therapy involves injection into a joint (intra-articular), that’s typically clinician-performed. At home, most people should stick to SubQ sites unless specifically directed and trained by a medical professional.
Step 4) Clean the skin correctly
- Use an alcohol swab to clean a circle larger than the injection area.
- Let the skin air-dry fully. (Injecting through wet alcohol can sting more.)
Step 5) Prepare the dose (prefilled vs vial)
If you have a prefilled syringe: keep the needle sterile and remove the cap only when ready to inject.
If you’re drawing from a vial (only if instructed):
- Swab the rubber stopper with alcohol and let it dry.
- Draw the exact prescribed amount.
- Follow your training for handling air bubbles.
If you need help converting vial strength + water volume into a draw amount per dose, use the Peptide Calculator to eliminate guesswork.
Step 6) Inject (SubQ technique)
- Pinch a fold of skin and fat at the chosen site.
- Hold the syringe steady.
- Insert the needle smoothly using the technique your clinician taught you.
- Inject slowly and steadily.
- Withdraw the needle smoothly.
- Apply gentle pressure with gauze for 10–20 seconds.
What it should feel like: usually a quick pinch or mild sting. If you consistently feel sharp pain, burning, or “bad injections,” ask your provider to review your technique and site selection.
Step 7) Dispose of sharps immediately
Place the used syringe/needle straight into a sharps container. Do not reuse needles or syringes—ever. Keep disposal simple: inject, drop, done.
Step 8) Log the shot (optional, but highly recommended)
Biohacking works best when you track what you’re doing. A simple log helps you catch patterns early:
- Date/time
- Injection site
- Dose
- Any immediate reactions
- Sleep, appetite, energy changes over the next 24–48 hours
Aftercare: What’s Normal vs. What’s a Red Flag
Common, mild reactions
- Mild redness or tenderness at the injection site
- A small temporary bump under the skin
- Light bruising
Potential side effects you may notice (varies by peptide)
- Nausea(often early on)
- Water retention or puffiness
- Changes in appetite or energy(especially with peptides affecting growth hormone pathways)
When to contact your provider
- Increasing redness, warmth, swelling, or pain after 24–48 hours
- Drainage/pus, fever, or feeling unwell
- Rash, itching, widespread hives, dizziness, or breathing difficulty
- Persistent lumps or irritation that worsens over time
Common Mistakes (And How to Avoid Them)
- Not letting alcohol dry: increases sting and irritation.
- Reusing needles/syringes: increases contamination risk and tissue trauma.
- Injecting the same spot repeatedly: causes irritation and lumps—rotate sites.
- Rushing the injection: inject slowly for comfort and consistency.
- Storing peptides incorrectly: follow the label; temperature matters.
- Taking internet protocols as “medical truth”: use your clinician + your data, not hype.
FAQ: How to Take a Peptide Shot
1) Do peptide shots hurt?
Most SubQ injections feel like a quick pinch. Consistent pain usually comes from injecting too fast, injecting into irritated tissue, or not rotating sites.
2) Where is the best place to inject peptides?
Common SubQ sites are the abdomen (away from the navel), outer thigh, and upper arm. Rotate sites to reduce irritation.
3) SubQ vs IM — how do I know which one I’m supposed to do?
Your prescription and clinician instructions should specify the route. If it’s unclear, don’t guess—ask for clarification or a quick injection walk-through.
4) What if I see a lump under the skin after injecting?
A small temporary bump can happen with SubQ injections. Rotate sites, avoid injecting into existing lumps, and monitor. If the lump is hot, expanding, very painful, or associated with fever, contact your provider.
5) Can I reuse an insulin syringe or needle?
No. Reuse increases infection risk and causes more tissue damage. Always use new sterile supplies.
6) How do I calculate how much to draw up?
Use the Peptide Calculator to convert vial amount + diluent volume into a consistent draw amount per dose. If you’re still unsure, confirm with your clinician or pharmacist.
7) What side effects should I watch for?
Common issues include mild injection-site redness/tenderness, nausea, water retention, and appetite/energy changes. Seek urgent help for breathing difficulty, facial/throat swelling, or severe infection signs.
8) Are peptide injections legal and regulated?
Rules vary by compound and context. If you’re trying to understand the difference between legitimate compounding rules and “gray market” claims, read: What Peptides Can Compounding Pharmacies Legally Sell in 2025?
Want Help Getting It Right the First Time?
If you want a clinician-style walkthrough on reconstitution, dosing math, and injection basics (without guesswork), explore:
For guides, calculators, and educational resources, browse the Project Biohacking Digital Library and subscribe to the Project Biohacking Newsletter.
FAQs
Do peptide shots hurt?
Most SubQ injections feel like a quick pinch. If it consistently hurts, it’s usually technique, speed, site choice, or injecting into irritated tissue.
Where is the best place to inject peptides?
For SubQ, common sites are the abdomen (away from the belly button), outer thigh, and upper arm. Rotate sites to reduce irritation.
SubQ vs IM: how do I know which one I’m supposed to do?
Your prescription/clinic instructions should say. If it’s unclear, don’t guess—ask. IM injections require different technique and needle selection.
What side effects should I watch for?
Mild redness/tenderness is common. Watch for nausea, water retention, appetite/energy changes, and any unusual mood/sleep changes. Seek urgent help for breathing difficulty, facial/throat swelling, or severe infection signs.
Can I reuse needles if it’s “just me”?
No. Reuse increases contamination risk and tissue damage. Use a new sterile needle and syringe every time.
What if I miss a dose?
Don’t double up unless your clinician specifically instructs it. Contact your provider for the correct next step.
How do I store peptide injections?
Follow the pharmacy label exactly. Many require refrigeration, but storage varies by product. Improper storage can reduce potency.