Peptide Therapy for Weight Loss: A Science-Backed Approach to Sustainable Results
How GLP-1 Agonists Like Semaglutide and Tirzepatide Target Metabolism for Sustainable Fat Loss

Weight loss remains one of the most challenging health goals for millions of people. Despite consistent effort with diet and exercise, many individuals struggle to achieve lasting results. Peptide therapy has emerged as a targeted solution that works with your body's natural biology rather than against it.
This approach uses specific amino acid chains to influence metabolism, appetite regulation, and fat oxidation. Unlike stimulant-based weight loss products or restrictive diets that often lead to rebound weight gain, peptides for weight loss target the underlying hormonal and metabolic pathways that govern body composition.
Understanding How Peptides Work in Your Body
Peptides are short sequences of amino acids that function as signaling molecules throughout your body. They communicate instructions between cells, triggering specific biological responses. In the context of weight management, certain peptides can activate receptors that control hunger, enhance fat burning, and improve metabolic efficiency.
Your body already produces numerous peptides naturally. Therapeutic peptides used for weight loss are typically synthetic versions of these naturally occurring compounds, designed to amplify specific beneficial effects. Because they mimic your body's own chemistry, they tend to integrate smoothly with existing physiological processes.
The mechanism varies depending on which peptide you use. Some stimulate growth hormone release, which plays a central role in maintaining lean muscle mass while promoting fat metabolism. Others act as GLP-1 receptor agonists, meaning they bind to receptors in your brain and digestive system that regulate satiety and glucose metabolism.
If you want a deeper breakdown of how these drugs function, including mechanism, safety profile, and drug-class comparisons, see our full guide to GLP-1 receptor agonists for weight loss.
Learn the Basics First
GLP-1 agonists are only one small piece of a much larger peptide landscape. To understand how different peptides work in the body and why peptide therapy includes more than weight-loss drugs, see our overview on what are peptides. To understand how peptide protocols extend beyond weight loss alone, review our complete overview of peptide therapy protocols and applications.
Key Peptides Used for Weight Management
Semaglutide: The GLP-1 Breakthrough
Semaglutide has transformed the landscape of medical weight loss. Originally developed for type 2 diabetes management, this peptide mimics glucagon-like peptide-1, a hormone your intestines produce after eating. When semaglutide activates GLP-1 receptors, several beneficial changes occur simultaneously.
Your brain receives stronger signals of fullness, reducing the urge to overeat. The rate at which food leaves your stomach slows down, extending the sensation of satiety between meals. Your pancreas responds more effectively to blood sugar fluctuations, releasing insulin more efficiently. These combined effects create an environment conducive to consistent fat loss.
Clinical trials have demonstrated impressive outcomes. Participants using semaglutide lost an average of 15% of their initial body weight over 68 weeks when combined with lifestyle modifications. That represents significantly better results than what most people achieve through diet and exercise alone.
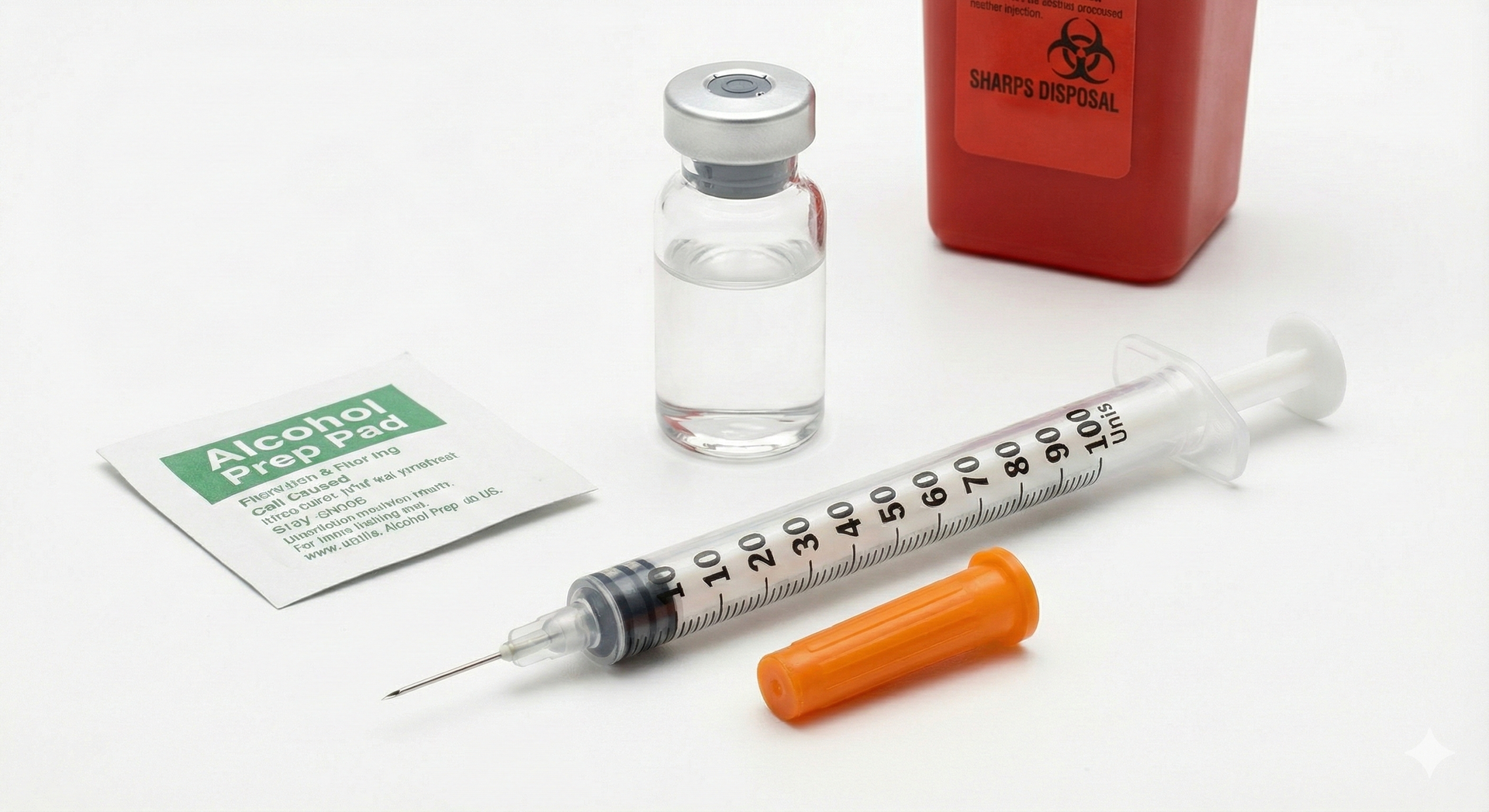
The peptide is administered once weekly via subcutaneous injection. Healthcare providers typically start patients on a low dose and gradually increase it over several weeks, allowing your body to adapt and minimizing potential side effects.
Tirzepatide: Dual-Action Innovation
Tirzepatide represents the next evolution in peptide therapy. While semaglutide targets only GLP-1 receptors, tirzepatide activates both GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) receptors. This dual mechanism creates a more comprehensive metabolic effect.
The addition of GIP receptor activation enhances insulin secretion and may improve how your body stores and processes nutrients. Early research suggests this dual approach might produce even more substantial weight reductions than single-agonist peptides, though individual responses vary.
Like semaglutide, tirzepatide helps control appetite and extends feelings of fullness. The improved insulin sensitivity benefits not just weight loss but overall metabolic health, making it particularly valuable for individuals dealing with obesity and prediabetes or type 2 diabetes.
Tesamorelin: Growth Hormone Pathway
Tesamorelin takes a different approach by stimulating your pituitary gland to release more growth hormone. This matters for weight loss because growth hormone influences how your body partitions nutrients between fat storage and muscle building.
Higher growth hormone levels promote lipolysis, the breakdown of stored fat for energy. They also support lean muscle preservation, which is crucial during caloric restriction. Maintaining muscle mass keeps your metabolic rate higher, making it easier to sustain weight loss long-term.
This peptide has been particularly studied in individuals with lipodystrophy, but its applications extend to broader weight management contexts when prescribed appropriately by qualified providers.
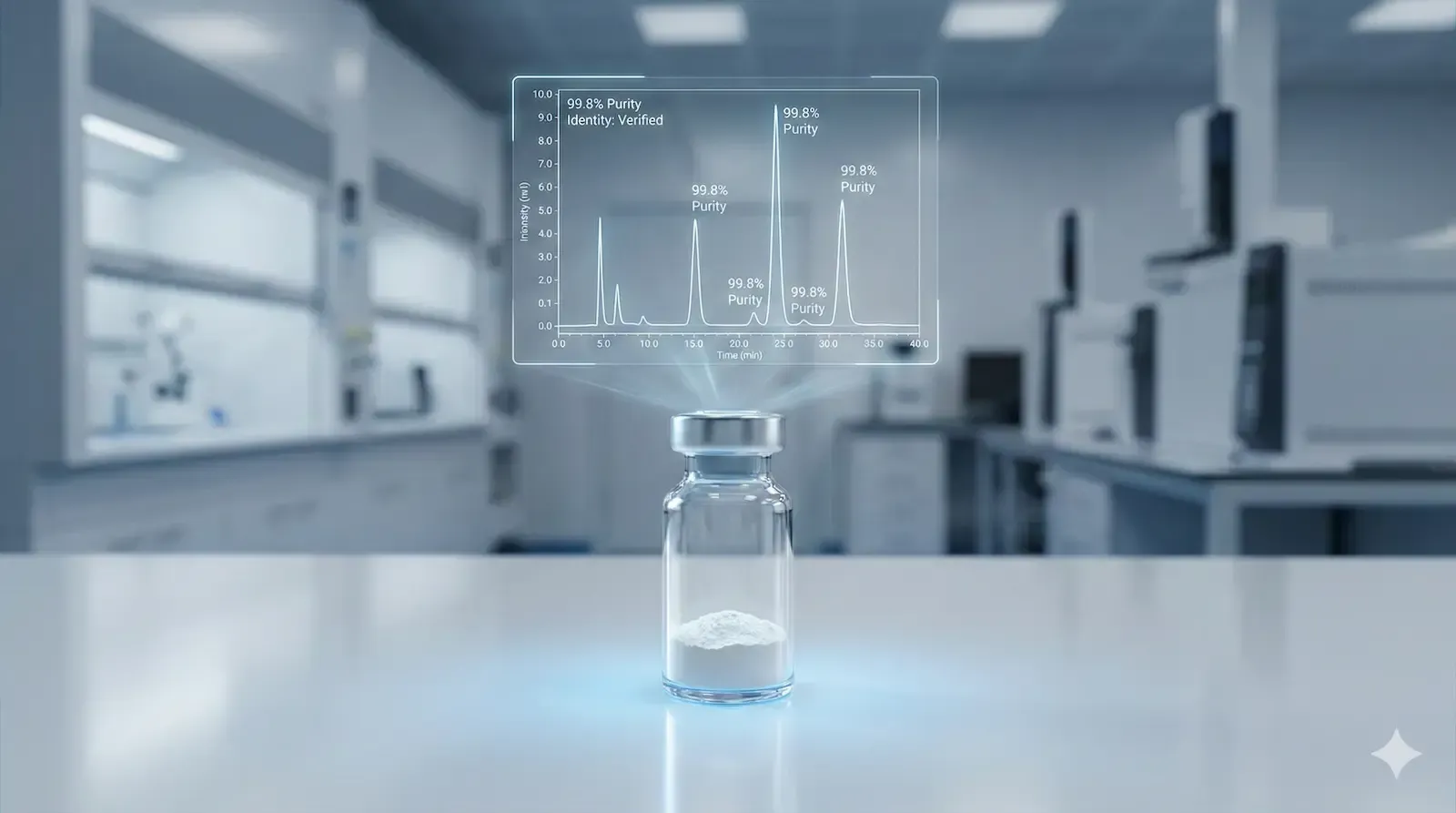
Biolongevity Labs offers several peptides commonly used in metabolic and body composition research. We track the current verified Biolongevity Labs discount code alongside updated documentation and third-party testing notes.Their product line includes both standalone peptides and ready-to-use formulations, each with updated certificates of analysis and transparent sourcing documentation. Always verify product suitability for your specific research goals before ordering.
Where GLP-1 Agonists Fit Within Peptide Therapy (and Where They Don’t)
GLP-1 agonists such as semaglutide and tirzepatide are pharmaceutical peptides used specifically for blood-sugar regulation and weight loss. While they are peptides by definition, they represent one narrow category within a much broader peptide landscape.
Peptide therapy, in a broader educational sense, includes many different peptides involved in metabolism, signaling, recovery, and cellular communication. These non-GLP-1 peptides are often discussed in research and coaching contexts for goals beyond weight loss alone.
This page discusses GLP-1 agonists as
one subset of peptide-based approaches, not as a definition of peptide therapy itself. Clinical treatment decisions involving prescription medications should always be made with a licensed medical provider, while
peptide therapy education encompasses a wider range of research-driven concepts and applications.
The Treatment Journey: What to Expect
Initial Assessment and Planning
Peptide therapy begins with a thorough medical evaluation. Your healthcare provider needs a complete picture of your health status, including current weight, body composition, metabolic markers, and any existing conditions that might influence treatment selection.
Blood work typically includes hormone panels, glucose and insulin markers, thyroid function, and lipid profiles. These baselines serve two purposes: they help identify the most appropriate peptide protocol for your situation, and they provide benchmarks for measuring progress.
Your provider will discuss your weight loss history, including previous attempts and their outcomes. This conversation helps identify patterns that might inform the treatment approach. Realistic goal-setting happens during this phase as well.
Customized Protocol Development
Based on your assessment results, your provider designs a peptide therapy protocol tailored to your physiology. This might involve a single peptide or, in some cases, a strategic combination. Dosing schedules are individualized, though most weight loss peptides are administered either daily or weekly through subcutaneous injection.
The injection technique is straightforward and can be self-administered at home after proper training. Most people inject into their abdomen, thigh, or upper arm. The needles used are very fine, similar to what people with diabetes use for insulin administration. If you are new to preparing injectable peptides, review our step-by-step peptide reconstitution guide before beginning.
Your treatment plan extends beyond peptide administration. Nutritional guidance helps you make food choices that complement the metabolic changes the peptides create. Exercise recommendations focus on maintaining muscle mass and maximizing fat oxidation.
Progress Monitoring and Adjustments
Regular follow-up appointments allow your provider to track your response to therapy. Weight and body composition measurements reveal whether you're losing fat while preserving muscle. Blood work monitors metabolic markers and ensures the therapy isn't causing any concerning changes.
Side effect management is an ongoing consideration. Most people tolerate peptides for weight loss well, but some experience gastrointestinal effects as their body adjusts. Your provider can modify dosing or suggest supportive measures to minimize discomfort while maintaining therapeutic benefit.
Adjustments to your protocol might include dose changes, switching to a different peptide, or modifying the lifestyle components of your plan. This flexibility ensures you continue progressing toward your goals even if initial approaches need refinement.
Expected Weight Reductions and Timeline
Results from peptide therapy vary based on starting weight, metabolic health, adherence to the protocol, and individual biological factors. However, patterns emerge from both clinical data and real-world use.
Many people notice appetite changes within the first week or two. Food cravings diminish, and you feel satisfied with smaller portions. This makes adhering to nutritional guidelines significantly easier than it would be through willpower alone.
Measurable weight loss typically becomes apparent in the first month. Initial drops may be more dramatic, particularly for individuals carrying excess fluid weight. As therapy continues, fat loss becomes the primary driver of weight reduction.
Over three to six months, cumulative weight loss of 10 to 15 pounds is common, though some individuals lose considerably more depending on their starting point and other factors. Importantly, much of this weight comes from visceral fat, the metabolically harmful fat surrounding your organs. Reducing visceral fat improves metabolic health markers even beyond what the scale shows.
The pattern of loss differs from crash dieting. Instead of rapid drops followed by plateaus and regain, peptide therapy tends to produce steady, consistent reductions. This gradual approach is metabolically healthier and more likely to result in lasting change.
Metabolic Benefits Beyond the Scale
While weight loss is the primary goal, peptide therapy creates metabolic improvements that extend beyond body composition. Understanding these broader effects helps explain why this approach supports long-term health better than weight loss methods that rely solely on caloric restriction.
Insulin sensitivity often improves significantly during peptide therapy. When your cells respond more effectively to insulin, your pancreas doesn't need to produce as much to manage blood sugar. This reduces strain on your metabolic system and lowers your risk of progressing to type 2 diabetes.
Inflammation markers frequently decrease as visceral fat reduces. Visceral fat produces inflammatory compounds that contribute to chronic disease risk. As you lose this harmful fat tissue, systemic inflammation tends to decline, potentially benefiting cardiovascular health, joint comfort, and overall wellbeing.
Many people report improved energy levels as their metabolism optimizes. Better blood sugar control means fewer energy crashes throughout the day. Enhanced sleep quality, which some peptides support indirectly through improved metabolic health, further contributes to feeling more energetic and focused.
The Critical Role of Protein Intake
Adequate protein consumption becomes especially important during peptide therapy. As your body loses weight, you want to ensure that loss comes primarily from fat tissue rather than muscle. Protein provides the amino acids necessary for maintaining and even building muscle mass.
Muscle tissue is metabolically active, meaning it burns calories even at rest. Preserving muscle keeps your metabolic rate higher, making it easier to maintain your weight loss after completing therapy. Losing muscle along with fat would leave you with a slower metabolism, setting you up for potential regain.
Protein also enhances satiety. While peptides like semaglutide and tirzepatide already reduce appetite through hormonal mechanisms, protein reinforces this effect through different pathways. Meals containing adequate protein keep you feeling satisfied longer.
Target protein intake during peptide therapy typically ranges from 0.7 to 1 gram per pound of your target body weight daily. High-quality sources include lean meats, fish, eggs, Greek yogurt, cottage cheese, legumes, and protein supplements if needed to meet your goals.
Distribute protein throughout your day rather than concentrating it in one meal. Your body can only process so much protein at once for muscle maintenance. Spreading intake across three to four meals optimizes utilization.
Understanding GLP-1 and GIP Agonists
The term "agonist" appears frequently in discussions of weight loss peptides. Understanding what this means helps you grasp how these therapies work.
An agonist is any substance that binds to a receptor and activates it, triggering a specific cellular response. Think of receptors as locks and agonists as keys that fit those locks and turn them. When a GLP-1 agonist like semaglutide binds to GLP-1 receptors, it activates the same pathways that natural GLP-1 would activate.
GLP-1 receptors exist in several locations throughout your body. In your brain, particularly in the hypothalamus, they influence appetite and satiety signals. In your pancreas, they regulate insulin secretion. In your stomach, they affect how quickly food moves through your digestive system.
By activating these receptors more strongly and for longer periods than natural GLP-1 does, therapeutic agonists create sustained effects that support weight loss. Your brain receives consistent signals to reduce food intake. Your blood sugar remains more stable. Your stomach empties more slowly, keeping you full between meals.
GIP agonists work similarly but target different receptors. GIP, like GLP-1, is an incretin hormone involved in glucose and energy metabolism. When tirzepatide activates both GLP-1 and GIP receptors simultaneously, it may produce synergistic effects that exceed what either pathway alone could achieve.
Managing Common Side Effects
Most people tolerate peptides for weight loss well, but some experience side effects, particularly when starting therapy or increasing doses. Understanding what to expect and how to manage these effects helps you stay comfortable while your body adapts.
Nausea
Nausea ranks among the most commonly reported side effects of GLP-1 agonists. It occurs because these peptides slow gastric emptying, the rate at which food leaves your stomach. While this effect contributes to increased fullness and reduced appetite, it can initially feel uncomfortable.
The good news is nausea typically diminishes within a few weeks as your body adjusts. Starting with a lower dose and gradually increasing it, as most protocols specify, significantly reduces the likelihood of severe nausea.
If you experience nausea, eat smaller, more frequent meals rather than large portions. Avoid fatty or spicy foods that might aggravate your stomach. Stay hydrated with small sips of water throughout the day. Ginger tea or ginger supplements may provide relief.
Let your provider know if nausea persists or becomes severe. They can adjust your dose or recommend additional supportive measures.
Digestive Changes
Some people experience changes in bowel patterns during peptide therapy. Diarrhea can occur as peptides increase gastrointestinal motility. Alternatively, constipation sometimes develops, possibly related to reduced food intake or changes in gut motility patterns.
For diarrhea, ensure you stay well hydrated and consider adding soluble fiber to help firm stools. Avoid caffeine and foods that might aggravate loose bowels. If symptoms persist beyond a few days, consult your provider.
Managing constipation involves increasing water intake, adding fiber-rich foods like vegetables and whole grains, and staying physically active. Movement helps stimulate normal digestive function. If dietary changes don't resolve the issue, your provider can recommend safe over-the-counter options or adjust your therapy.
Other Considerations
Fatigue occasionally occurs during the initial adjustment period, though it usually resolves as your body adapts. Ensure you're eating enough to fuel your activity level, staying hydrated, and getting adequate sleep.
Injection site reactions—mild redness, swelling, or tenderness where you inject—are generally minor and temporary. Rotating injection sites and using proper technique minimizes these effects.
Serious side effects are rare but require immediate medical attention. These include severe abdominal pain, signs of pancreatitis, significant changes in heart rate, or allergic reactions. Your provider will discuss warning signs to watch for.
Who Benefits Most from Peptide Therapy
Peptide therapy for weight loss isn't appropriate for everyone, and it's not meant to replace healthy lifestyle habits. It works best as part of a comprehensive approach for specific populations.
Individuals with a body mass index of 30 or higher often see substantial benefits. For those with a BMI of 27 or higher who have weight-related health conditions like high blood pressure, type 2 diabetes, or elevated cholesterol, peptide therapy may offer particular value.
People who have struggled to lose weight through diet and exercise alone despite genuine effort often find peptide therapy provides the metabolic boost needed to overcome barriers. This doesn't mean peptides replace the need for healthy eating and physical activity, but rather that they make these behaviors more effective.
Those dealing with metabolic issues such as insulin resistance or prediabetes may benefit from peptides that improve insulin sensitivity while supporting weight loss. The dual benefit addresses both the weight concern and the underlying metabolic dysfunction.
Peptide therapy may not be suitable for pregnant or breastfeeding women, individuals with certain types of thyroid cancer or family histories of specific endocrine conditions, or people with severe gastrointestinal disorders. A thorough medical evaluation determines candidacy.
Combining Peptides with Lifestyle Optimization
The most successful outcomes occur when peptide therapy supports, rather than replaces, healthy lifestyle habits. Think of peptides as tools that make proper nutrition and exercise more effective by optimizing your metabolic environment.
Nutritional strategies should focus on whole, minimally processed foods. Emphasize lean proteins, fibrous vegetables, and moderate amounts of complex carbohydrates and healthy fats. The appetite suppression peptides provide makes it easier to follow these guidelines without feeling deprived.
Resistance training becomes particularly valuable during peptide therapy. Building or maintaining muscle mass offsets any metabolic slowdown that weight loss might cause. Aim for at least two to three sessions weekly that target all major muscle groups.
Cardiovascular exercise supports fat oxidation and cardiovascular health. Moderate-intensity activities like brisk walking, cycling, or swimming for 30 to 45 minutes most days of the week complement peptide therapy well. High-intensity interval training can be incorporated if appropriate for your fitness level.
Sleep quality matters more than many people realize for weight management. Poor sleep disrupts hunger hormones, increases cravings, and impairs insulin sensitivity. Aim for seven to nine hours of quality sleep nightly.
Stress management techniques like meditation, deep breathing, or yoga help regulate cortisol, a hormone that can promote fat storage when chronically elevated. Finding healthy ways to manage stress supports your overall weight loss effort.
Long-Term Maintenance and Sustainability
Peptide therapy typically continues for several months to a year or more, depending on your goals and response. As you approach your target weight, the focus shifts toward maintaining your results.
Some people transition off peptides once they've achieved their goals and successfully adopted the lifestyle habits needed to maintain their weight. Others continue with maintenance dosing to support long-term weight stability, particularly if they have struggled with regain in the past.
The habits you build during therapy—eating adequate protein, staying physically active, managing stress, sleeping well—become the foundation for lasting success. Peptides create the metabolic conditions that make developing these habits easier, but ultimately, your behaviors determine whether results endure.
Regular monitoring continues even after completing active therapy. Checking in with your provider, tracking your weight and body composition, and staying attuned to how you feel helps you catch any backsliding early when it's easiest to address.
View peptide therapy as a catalyst for lasting change rather than a temporary fix. The metabolic improvements and habit formation that occur during treatment create momentum that carries forward, increasing your chances of maintaining your results long-term.
Making an Informed Decision
If you're considering peptide therapy for weight loss, start with a thorough evaluation from a qualified healthcare provider experienced in this field. Come prepared with your complete medical history, information about previous weight loss attempts, and clear goals for what you hope to achieve.
Ask questions about which peptide might suit your situation best, what the full protocol involves beyond injections, what side effects to anticipate, and what success looks like in your specific case. Understanding both the potential benefits and limitations helps you make an informed choice.
Consider the commitment involved. Peptide therapy requires regular injections, ongoing monitoring, lifestyle modifications, and typically several months of consistent effort. If you're ready to make that investment in your health, the results can be transformative.
Verify that your provider offers comprehensive support, not just prescriptions. The most effective programs include nutritional guidance, exercise recommendations, regular monitoring, and adjustments based on your response. This holistic approach maximizes your chances of success. Understanding how to evaluate certificates of analysis and lab transparency is critical. Our breakdown of third-party testing for peptides explains what actually matters when assessing supplier quality.
Peptide therapy represents a significant advancement in weight management, offering a science-backed option for people who need more than willpower alone. When used appropriately under medical supervision as part of a comprehensive plan, it can help you achieve and maintain the healthy weight you've been working toward.
How long does it take to see results from peptide therapy for weight loss?
Most people notice appetite changes within the first one to two weeks. Measurable weight loss typically becomes apparent within the first month, with continued steady progress over subsequent months. Individual timelines vary based on starting weight, metabolism, adherence to protocol, and which peptide is used.
Can I stop taking weight loss peptides once I reach my goal weight?
Some individuals successfully maintain their weight loss after discontinuing peptides by sustaining the lifestyle changes they developed during therapy. Others benefit from maintenance dosing to support long-term weight stability. Your provider will help determine the best approach for your situation based on your weight loss history and risk of regain.
Are peptides for weight loss safe for long-term use?
Clinical trials have studied peptides like semaglutide for extended periods, demonstrating acceptable safety profiles when used under medical supervision. Long-term safety continues to be monitored through ongoing research. Regular medical monitoring throughout treatment helps identify any concerns early.
How much weight can I realistically lose with peptide therapy?
Weight loss varies significantly between individuals. Clinical studies show average reductions of 10 to 15% of initial body weight over several months, though some people lose more or less. Factors influencing results include starting weight, metabolic health, adherence to lifestyle modifications, and individual response to the specific peptide used.
Do I still need to diet and exercise while using peptides for weight loss?
Yes. Peptides optimize your metabolic environment and reduce appetite, making healthy behaviors more effective and easier to maintain. However, they work best when combined with appropriate nutrition and regular physical activity. Think of peptides as tools that enhance your efforts rather than replacements for healthy lifestyle habits.
What happens if I experience side effects from weight loss peptides?
Most side effects are mild and temporary, resolving as your body adjusts. Your healthcare provider can modify your dosage, suggest management strategies, or switch to a different peptide if needed. Severe side effects are rare but require immediate medical attention. Maintaining open communication with your provider ensures side effects are addressed promptly.
Can peptide therapy help with stubborn fat that won't respond to diet and exercise?
Peptide therapy can be particularly effective for individuals who have plateaued despite consistent healthy behaviors. By targeting specific metabolic pathways, peptides may help overcome biological barriers to further fat loss. However, success still requires adherence to appropriate nutrition and exercise protocols alongside the therapy.